It is much more common than you might think, but when it appears it can cause great alarm.
Many people panic when they see blood in their stool or when they defecate and think they might have something serious, such as colon cancer.
However, there are other more frequent causes that may be behind this symptom, some more serious than others.
Fermín Mearín, director of the digestive system service at Centro Médico Teknon, in Spain, explained to BBC Mundo the most frequent causes:
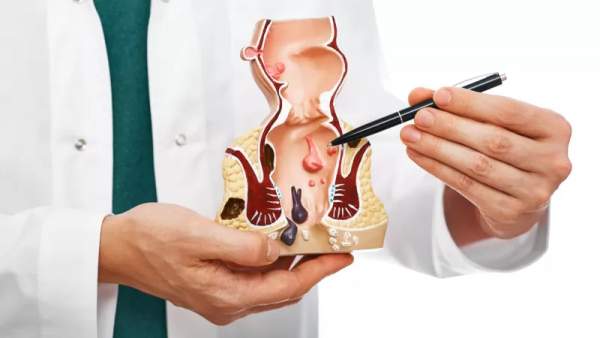
- hemorrhoids or anal fissure: they usually cause the presence of bright red blood, which may appear after bowel movements.
“This is usually indicative that the bleeding is coming from below and that the cause is in the anus or rectum,” says Dr. Mearin.
Hemorrhoids may not be observable to the naked eye, but they can be detected with a careful anal examination, by digital rectal examination and rectoscopy.
An anal fissure can also be detected with a simple examination. It is a small cut in the anus that can occur, for example, in people who suffer from constipation and can be very painful.
- Inflammatory bowel disease: the cause of the appearance of inflammatory lesions in the intestine can be ulcerative colitis or Crohn’s disease.
“In this case, in addition to inflammation there is usually diarrhea and abdominal pain,” says Mearín. They usually affect the colon, although Crohn’s disease sometimes affects the small intestine.
In this case, the stool is between red and dark, mixed color. “They are redder the lower down, near the anus, the inflammation is,” explains Mearín.

- On the other hand, if the stool is very black and sticky, it may indicate high bleeding in the stomach.
In this case, a gastroscopy should be performed to rule out the possibility of a bleeding ulcer in the stomach or duodenum.
In most cases, the appearance of blood does not mean that there is a serious cause.
But if the blood is dark and appears mixed with the stool, it is probably coming from the colon or somewhere farther away. In this case, doctors recommend a colonoscopy to check for colon polyps, colon cancer or vascular lesions.
In some countries there are colon cancer screening programs in which the population over a certain age is examined.

These programs use the detection of blood in the stool as an indicator of colon cancer risk.
If blood is detected in the patient’s stool, the patient is scheduled for retesting, which is often a source of distress for many.
In many cases, however, that distress is not justified by the statistics.
“People come to the office frightened, but most of the time they have benign pathologies,” says Mearín.
Being over 50 or having a family history of colon cancer usually causes doctors to choose to perform an endoscopy to see the condition of the colon.
And although the color of the stool is a useful guide, it should be taken into account that the ingestion of certain foods can also condition it.
Black licorice, for example, can cause black stools. And beets or tomatoes can sometimes cause reddish stools.
In any case, whenever blood is detected during a bowel movement, it is important to see a doctor promptly to obtain an accurate diagnosis.