If you have access to contraception today, it’s easy to take these advances for granted.
But it was only during the last century that a number of key discoveries changed women’s lives.
Before the invention of the modern intrauterine device (IUD), or hormonal contraceptives, most products used had little effect and were more useful in delaying pregnancy than preventing it.
When the contraceptive pill became available in the early 1960s, this marked a turning point.
Its very low failure rate of less than 1% when used correctly helped put control of contraception firmly in the hands of women.
While the Pill can have some serious side effects, for many women it still provides a much less uncomfortable experience than these methods that preceded it.
1. Reusable condoms
People have used condoms since at least the 17th century, primarily to prevent sexually transmitted infections.
Initially, these protectors were made of natural material such as animal intestines or linen.
Just a few years after the invention of synthetic rubber (1844), the rubber condom was developed.
It was designed to be rinsed and reused, and for that very reason was thicker and less comfortable than today’s male condoms.
The disposable latex condom was not invented until the 1930s.
These pads were thinner, more comfortable and, of course, only used once.
Later that decade, the U.S. judiciary overturned the ban on the sale of “immoral goods” and this helped condom use become more widespread.
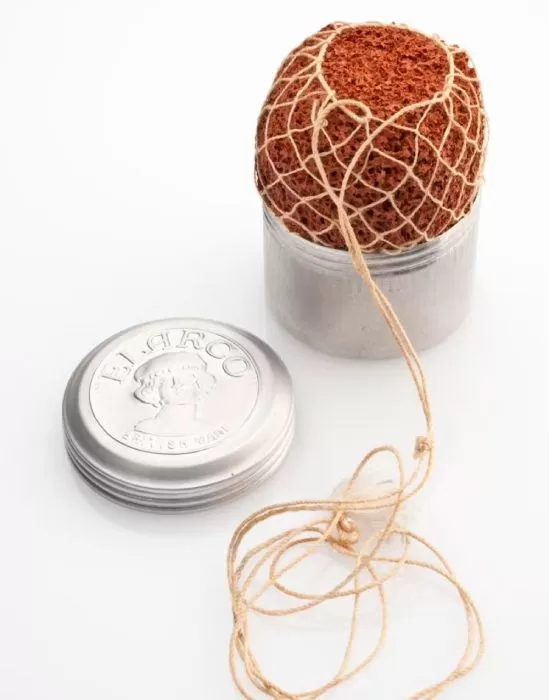
2. Acid soaked sponges
Since acid kills sperm, a traditional home contraceptive method was to insert a sponge soaked in vinegar into the vagina.
Sponges designed specifically for this use were commercially available in the early 20th century and contained spermicidal chemicals.
Some variations of the spermicidal sponge are still available. However, less than 1% of women in the UK use this type of sponge today.
The typical failure rate, particularly for younger women, is around 12% to 24% per year. In general, younger women are more likely to become pregnant when using less effective methods because they are more fertile than older women.
3. Diaphragms and caps
The diaphragm and its smaller cousin the cap were invented in the early 19th century.
Like condoms, they act as a physical barrier to sperm. Like mushrooms, they are used together with spermicide.
These products are inserted into the vagina before intercourse and must remain in place for at least six hours after intercourse in order for the spermicide to kill the sperm. Before World War II, caps and diaphragms were widely used in the United States and Europe.
But the typical failure rate with these methods for young women is about 12%. As a result, they are currently used by less than 1% of women worldwide.
Part of the reason barrier methods have a high failure rate is that they do not prevent a woman from ovulating. If the sperm can pass through the barrier, the chance of fertilization is high.
Another disadvantage is that they are difficult to insert and must be inserted before intercourse, a time when women can better think about other things.
4. Douching with antiseptic
Rinsing the vagina after intercourse, often with an antiseptic solution, was used as a method of contraception in the early 20th century.
Douching does not affect sperm that have already begun their journey through the cervix. Therefore, the efficacy of douching was very low.
Today, douching is strongly discouraged by health professionals because of the damage it causes to the vaginal flora (the vagina’s natural protective bacteria). The use of this method can cause vaginal irritation and infection.
5. IUD of silkworm gut
Intrauterine devices (IUDs) remain popular, but they did not always work in the same way as modern products.
Early intrauterine methods were based on the (partially correct) belief that any device placed inside the uterus would likely prevent a fertilized egg from implanting and developing.
In the 19th century, fork-shaped pessaries were used to prevent pregnancy.
These devices had two arms that protruded through the cervix into the vagina and a button that covered the cervix. It is hard to imagine that these products were comfortable.
Polish gynecologist Richard Richter published an article in 1909 about how he inserted a silkworm gut ring into a patient’s uterus, with two threads protruding to allow its removal.
At the time, many gynecologists discreetly used their own versions of these devices, due to laws against promoting contraception in many countries.
The so-called Graefenberg ring replaced the silkworm gut with a metal alloy ring in the 1920s.
German gynecologist Ernst Graefenberg first tried using pure silver, but the body absorbed the metal and women’s gums turned blue.
During the 1950s, 1960s and 1970s, all kinds of IUD materials and shapes were used, from foils to coils, until researchers realized that copper improved the devices’ effectiveness.
In the 1970s there were about 70 different intrauterine devices on the market in the United States.
One of those copper devices was the infamous Dalkon shield, which allowed bacteria to ascend into the uterus due to the design of the threads used to remove it. This caused a large number of infections and caused the acceptance of intrauterine methods to plummet in the 1970s.
Modern intrauterine devices (IUDs) are placed completely in the uterus, contain copper or hormones such as slow-release progesterone, and are much safer and more effective than older devices.
Infections due to IUDs are now rare, but do occur occasionally in the first few weeks after insertion.
Both hormonal and copper devices now have failure rates of less than 1%.
Today we have several methods of contraception that, if used correctly, rarely fail, but women still struggle to find the method that is best for them.
New research is focused on reducing the side effects of contraceptive methods.
